Steam Sterilizer
Stream sterilization achieves by exposing the items to sterilizing with saturated steam under pressure. Heat enhances the ability of heat to kill microorganisms by reducing the time and temperature required to denature or coagulate proteins in the microorganisms.
Working Principle
A basic principle is Gay Loussac’s law when the pressure of a gas increases the temperature increase proportionally. With about 15 pounds of pressure per square inch (psi), the temperature rises to 121oC. Increasing the pressure to 20 psi raises the temperature to 134oC.

Uses
An electric stream sterilizer uses steam to kill any germs. The sterilizer unit sits on your bench top and is plugged into the power socket like a toaster or electric kettle. You pour a small amount of water into the unit, put the cover on and the metal element at the bottom heats up, turning the water to steam.
- Steam flows through the sterilizer beginning the process of displacing the air.
- Exhaust valve will close, causing the interior temperature and pressure to ramp up to the desired setpoint.
- Desired temperature maintain until the desired time is reached.
- The pressure release from the chamber through an exhaust valve.
Parts
a. Chamber and jacket.
b. Thermostatic traps.
c. Vacuum system.
d. Steam generator.
Chamber and jacket
The chamber is the primary component of a steam sterilizer where the materials to be sterilized are placed and sterilization happens & the jacket is filled with steam, reducing the time that sterilization cycles take to complete and reducing condensation within the chamber.
Thermostatic traps
A device designed to allow air and water (condensate) to escape from the chamber. Steam traps are temperature sensitive valves that close when heated past a set point.
Vacuum system
Forcibly remove air by pulling a vacuum on the chamber before the cycle (also known as pre-vacuum), it also helps by pulling a vacuum after the cycle (also known as a post- vacuum) to remove the steam remaining in the chamber and dry off the goods inside the autoclave.
Article About:- Health & fitness
Article About:- Medical Technology
Article About:- Sports

Steam generator
Boilers are typical underneath the chamber to the sterilizer and utilize electric heating elements to heat water and generate steam.
1. Phase conditioning
a. Chamber closes with jacket.
b. Steam loaded.
c. Jacket pressure and chamber pressure displayed.
2. Heating conditioning
• Steam generated
3. Sterilization phase
• 121 C at 10 psi in 20 min
• 134 C at 20 psi in 5 min
4. Dry phase
• Removal of water
5. Aeration/Vent
• Releasing high pressure
• Use vacuum
How does an autoclave work
An autocleve is a device used to sterilize equipment and supplies by subjecting them to high pressure saturated steam at high temperatures. The primary mechanism by which an autoclave works is through a combination of heat, steam, and pressure.
Here’s a step-by-step explanation of how an autoclave works:
- Loading: The items to be sterilized, such as medical equipment, laboratory equipment, or other materials, are placed inside the autoclave chamber. It is important to ensure that items are arranged in a way that allows for proper steam circulation and thorough sterilization.
- Sealing: The autoclave chamber is sealed to create an airtight environment. This prevents steam from escaping during the sterilization process.
- Water Filling: Water is added to the autoclave’s reservoir or steam generator. The amount of water required is determined by the manufacturer’s guidelines and the capacity of the autoclave.
- Pre-vacuum (optional): In some autoclaves, a pre-vacuum cycle is performed prior to sterilization. It involves the removal of air from the chamber by creating a vacuum, which helps improve steam penetration and sterilization efficiency.
- Heating: The autoclave’s heating element raises the temperature of the water, producing steam. The heat source can be an electric coil, gas burner or heating jacket.
- Pressure: As the water heats up and turns into steam, the pressure inside the autoclave chamber begins to increase. The steam pushes the remaining air out of the chamber, ensuring effective sterilization.
- Sterilization phase: Once the desired temperature and pressure are reached, the autoclave maintains them for a predetermined period of time. The combination of high temperature, steam, and pressure destroys bacteria, viruses, fungi, and other microorganisms, making objects sterile.
- Depressurization: After the sterilization step, the pressure inside the autoclave is gradually reduced. This step is usually done slowly to prevent sudden temperature and pressure changes that could damage the sterilized items.
- Drying (optional): Some autoclaves provide a drying step to remove excess moisture from sterilized items. This helps prevent contamination and allows for immediate use or storage.
- Unloading: Once the drying step, if applicable, is complete, the autoclave chamber can be opened, and the sterilized items removed. It is important to handle items with care and follow proper protocols to maintain sterility.
Autoclaves are widely used in medical, dental, pharmaceutical, and laboratory settings to ensure the safety and sterility of equipment, surgical instruments, and supplies. The exact settings and procedures may vary depending on the specific autoclave model and the requirements of the items to be sterilized.
Article About:- Health & fitness
Article About:- Medical Technology
Article About:- Sports

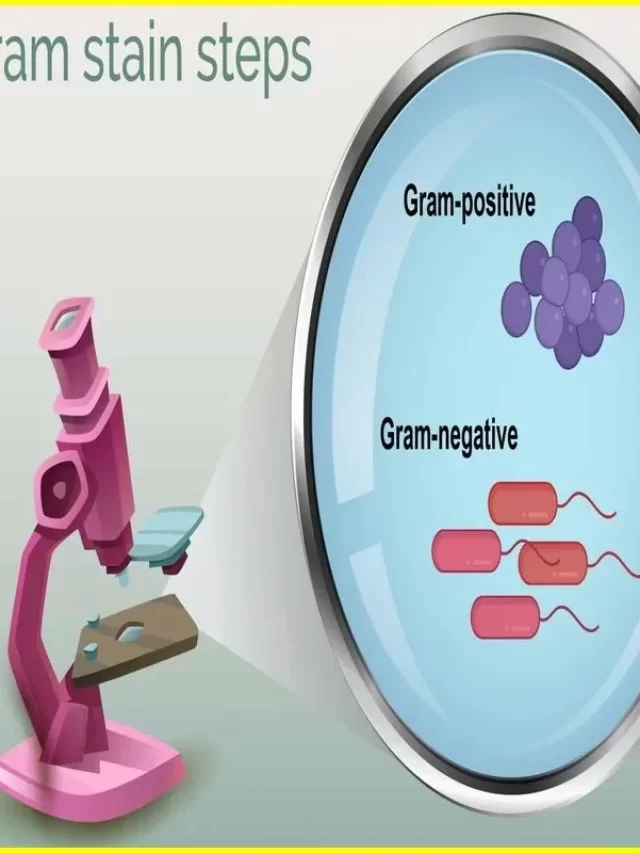
How does an autoclave kill microorganisms?
An autoclave kills microorganisms through a combination of high temperature, steam, and pressure. These factors work together to inhibit the vital functions of microorganisms and ultimately lead to their destruction. Here’s how an autoclave achieves microbial sterilization:
- High temperature: Autoclaves typically operate at temperatures from 121 to 134 °C (250 to 273 °F). This elevated temperature is much higher than the optimum growth temperature for most microorganisms. Exposure to high temperatures denatures proteins, disrupts cell membranes, and disrupts essential metabolic processes, effectively killing microorganisms.
- Steam: Autoclaves use saturated steam, meaning the steam is in equilibrium with liquid water at a certain temperature. Steam has the advantage of efficiently transferring heat energy to the objects to be sterilized, penetrating even small cracks and irregularities. Hot steam directly interacts with microorganisms and transfers heat, further contributing to their destruction.
- Pressure: Autoclaves create and maintain a high-pressure environment during the sterilization process. The pressure within the autoclave chamber is typically about 15 to 30 pounds per square inch (psi) above atmospheric pressure. The increased pressure raises the boiling point of water, causing it to reach higher temperatures before it evaporates. This elevated temperature, combined with the increased pressure, increases the effectiveness of sterilization by ensuring that heat reaches all areas of the object to be sterilized.
- Moist Heat: The combination of high temperature and steam in the autoclave creates a moist heat environment. Moist heat is particularly effective at killing microorganisms because it rapidly denatures proteins and disrupts essential cell structures. The moisture also helps hydrate the microorganisms, making them more vulnerable to the damaging effects of heat.
In an autoclave these factors of high temperature, steam and pressure work synergistically to kill microorganisms. The elevated temperature disrupts their cellular structures and essential biological processes, while the steam and pressure help ensure that the heat reaches all areas and the microorganisms are fully exposed to the sterilizing conditions.
It is important to note that autoclaves are highly effective against most microorganisms including bacteria, viruses, fungi and spores. However, some heat-resistant bacterial spores may require extended sterilization time or alternative methods to achieve complete sterilization.
FAQ
How must you label an autoclave package

When labeling an autoclave package, it is important to provide clear and specific information to ensure proper handling and identification of the contents.
Sterilization indicator.
Date and time.
Sterilization method.
What is an autoclave

An autocleve is a device that uses high-pressure and high-temperature steam to sterilize tools, equipment, and other items. It is commonly used in medical, dental, veterinary and laboratory settings to ensure the eradication of bacteria, viruses, fungi and other microorganisms.
What is an autoclave used for

An autocleve is used for sterilization, which is the process of eliminating or killing microorganisms, including bacteria, viruses, fungi, and spores, from equipment, instruments, and other objects.
Medical and healthcare settings: Autocleves are used to sterilize medical instruments, surgical tools, syringes, dressings, and other equipment to prevent the transmission of infections in hospitals, clinics, and laboratories.
Dental practices. ..
Laboratories. ..
Pharmaceutical industry. ..
Veterinary medicine. ..